When COVID-19 hit Minnesota, staff at Hennepin County’s Public Health Clinic (PHC) had to get creative – fast.
The downtown clinic, home to Red Door -- the state’s largest sexual health clinic – as well as tuberculosis and refugee health clinics, serves over 11,000 people per year on average.
In 2019, staff in the clinic completed 9,703 HIV tests; identified 1,033 gonorrhea and 1,365 chlamydia infections; offered direct observation therapy to 132 patients with tuberculosis; distributed 837 naloxone kits, which prevented an estimated 270 opioid overdoses, and more.
Three staff describe the new model that’s allowing them to serve clients safely.
The Hennepin County Public Health Clinic serves over 11,000 people per year. Now they’re doing it during COVID-19.
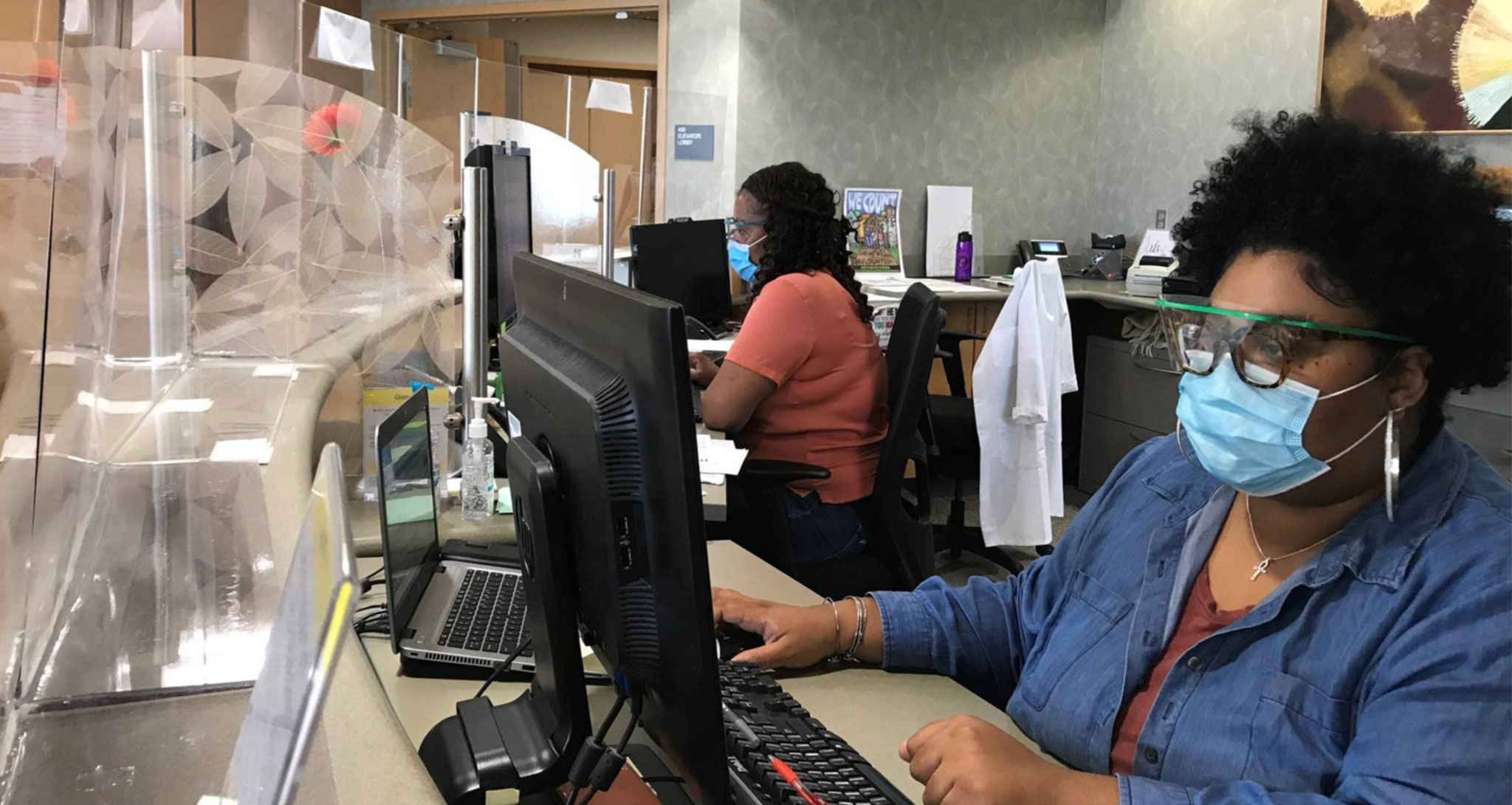
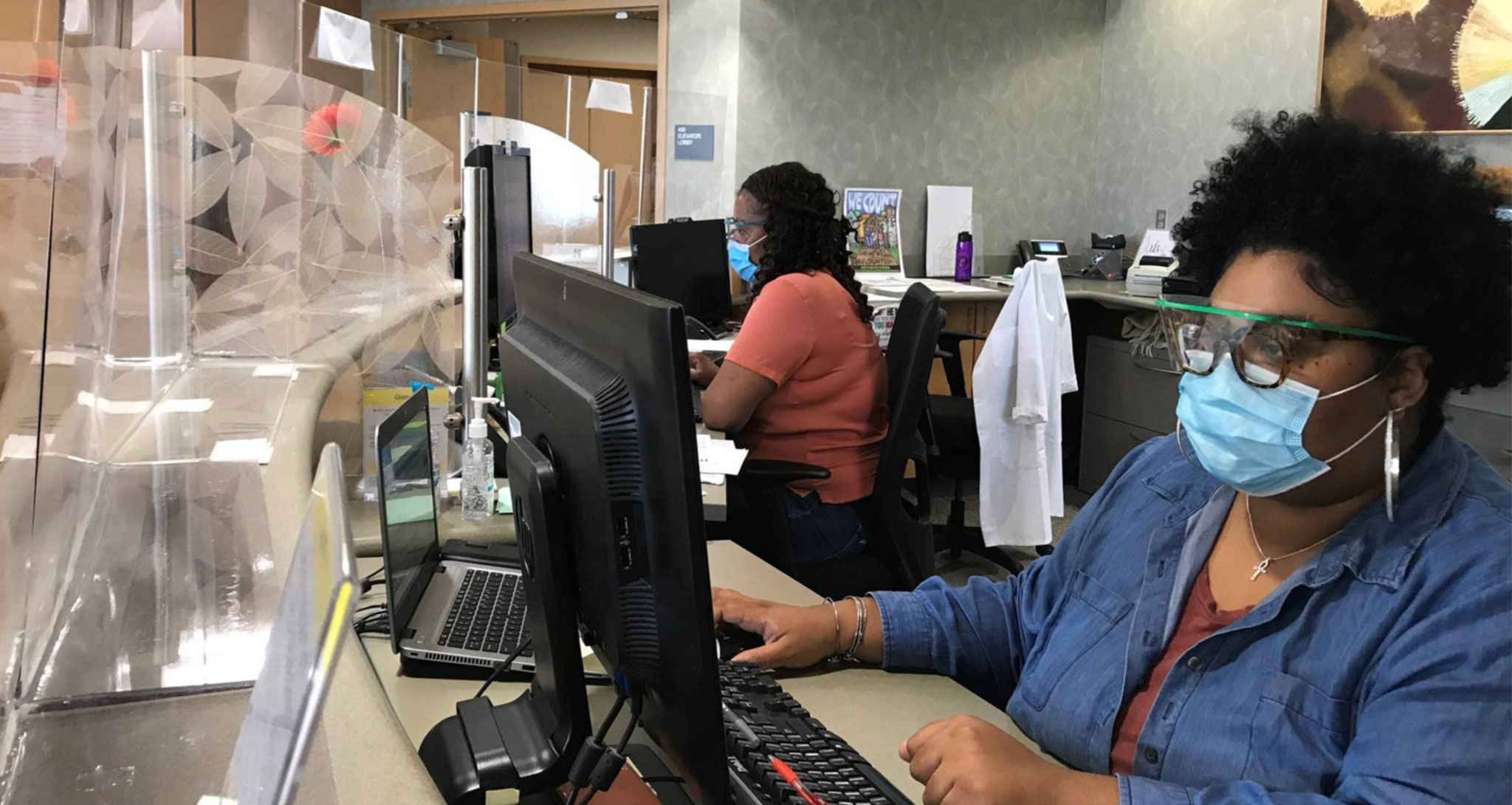
“Before COVID-19, we’d have 20 or 30 people in the Public Health Clinic lobby, and we realized we couldn’t do that anymore,” says Nurse Practitioner Ashley Beasley.
At the clinic, providers like Beasley begin their appointments by taking patients’ health histories and asking them questions about their current health issues. Since COVID-19, this part of the appointment is taking place by phone. If, after that initial consultation, providers determine that they can continue serving a client by phone, they do so.
But some things, like taking a physical sample to determine if you have a sexually transmitted infection, can’t be done over the phone. When these patients come to the clinic, they’re led straight to an exam room, instead of waiting in the lobby.
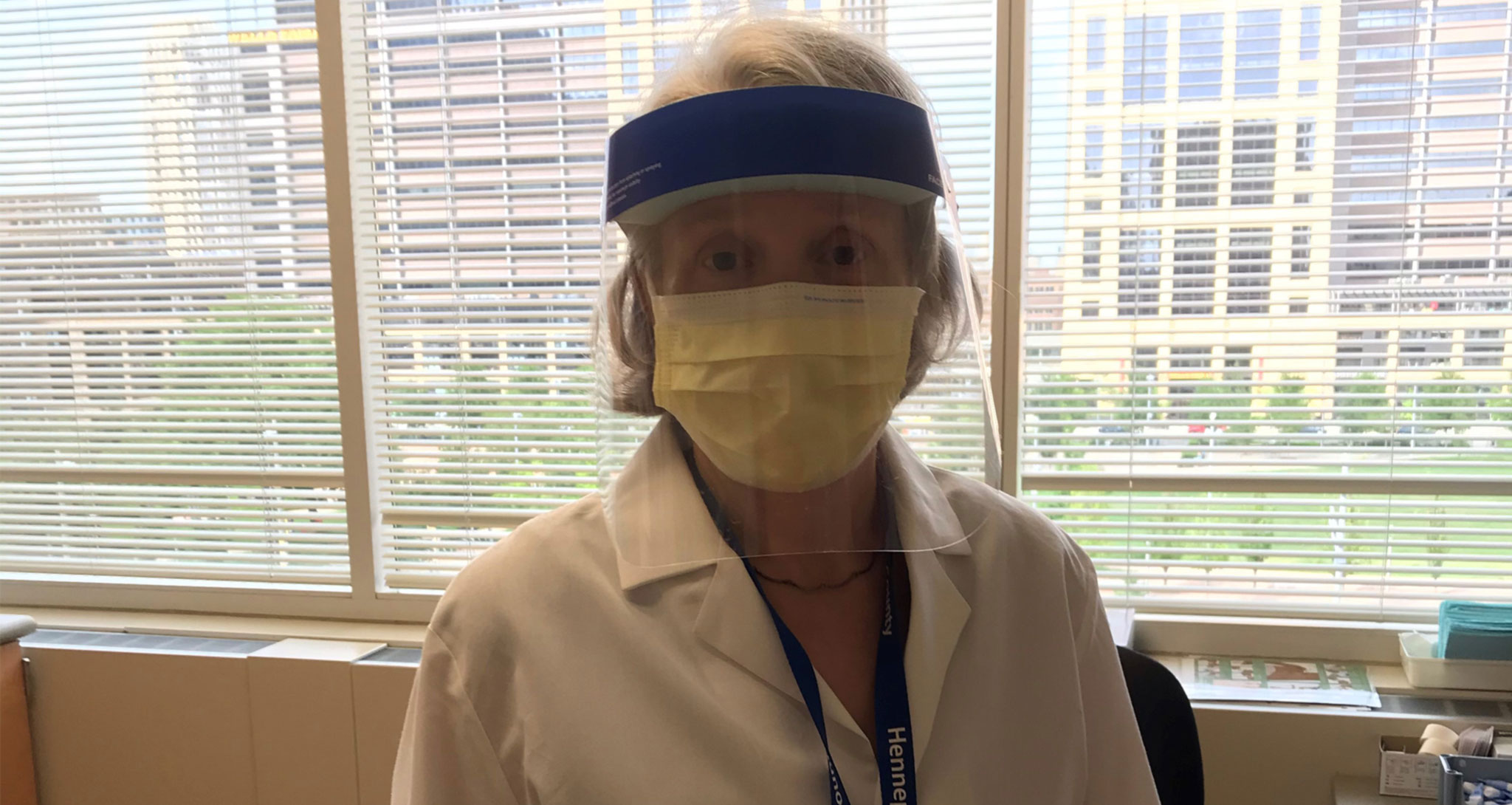
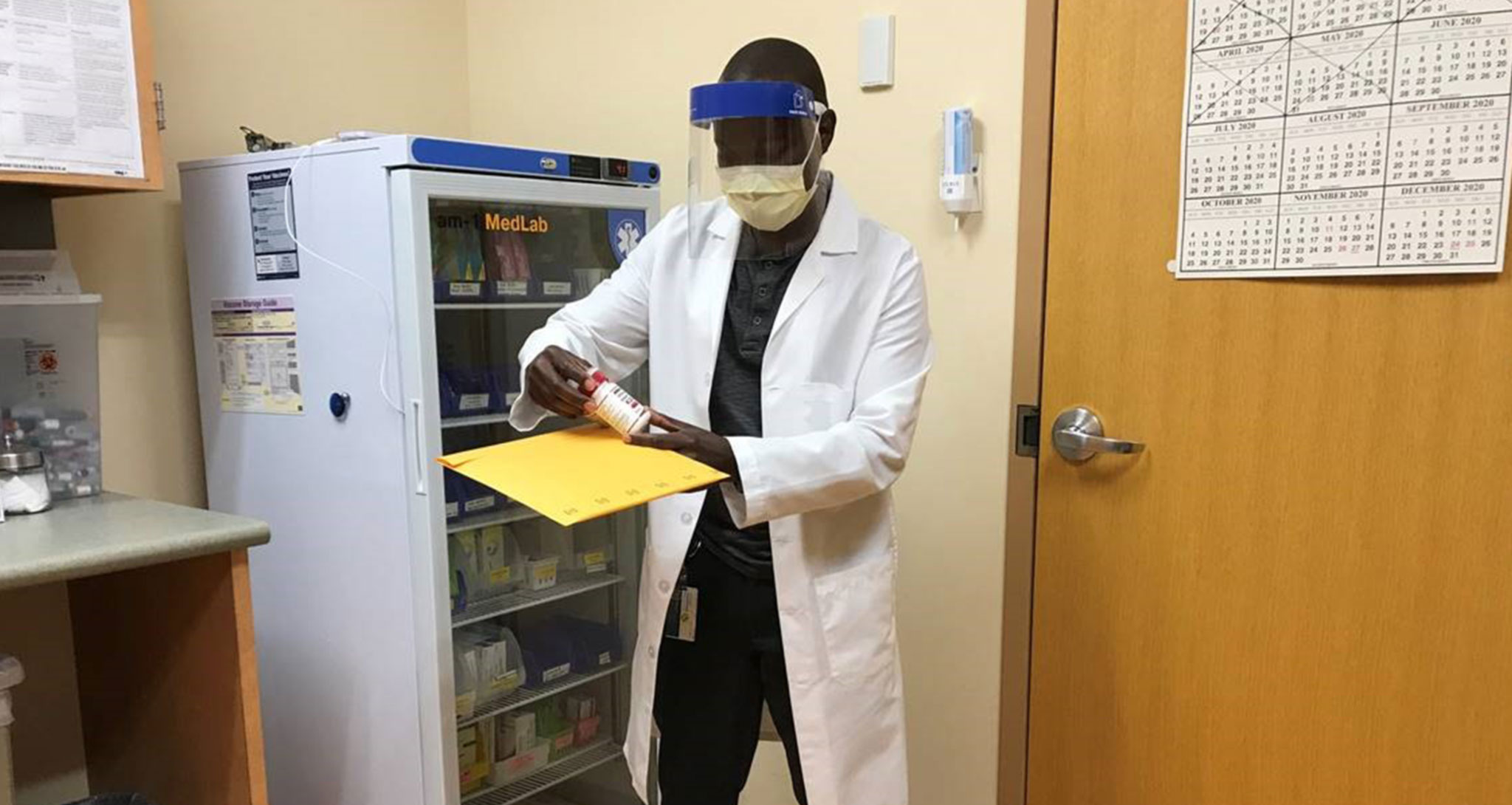
Staff are wearing masks and face shields and the exam rooms are thoroughly disinfected. “We’re modeling for our patients a new normal,” says Beasley.
The Public Health Clinic is now offering telehealth.
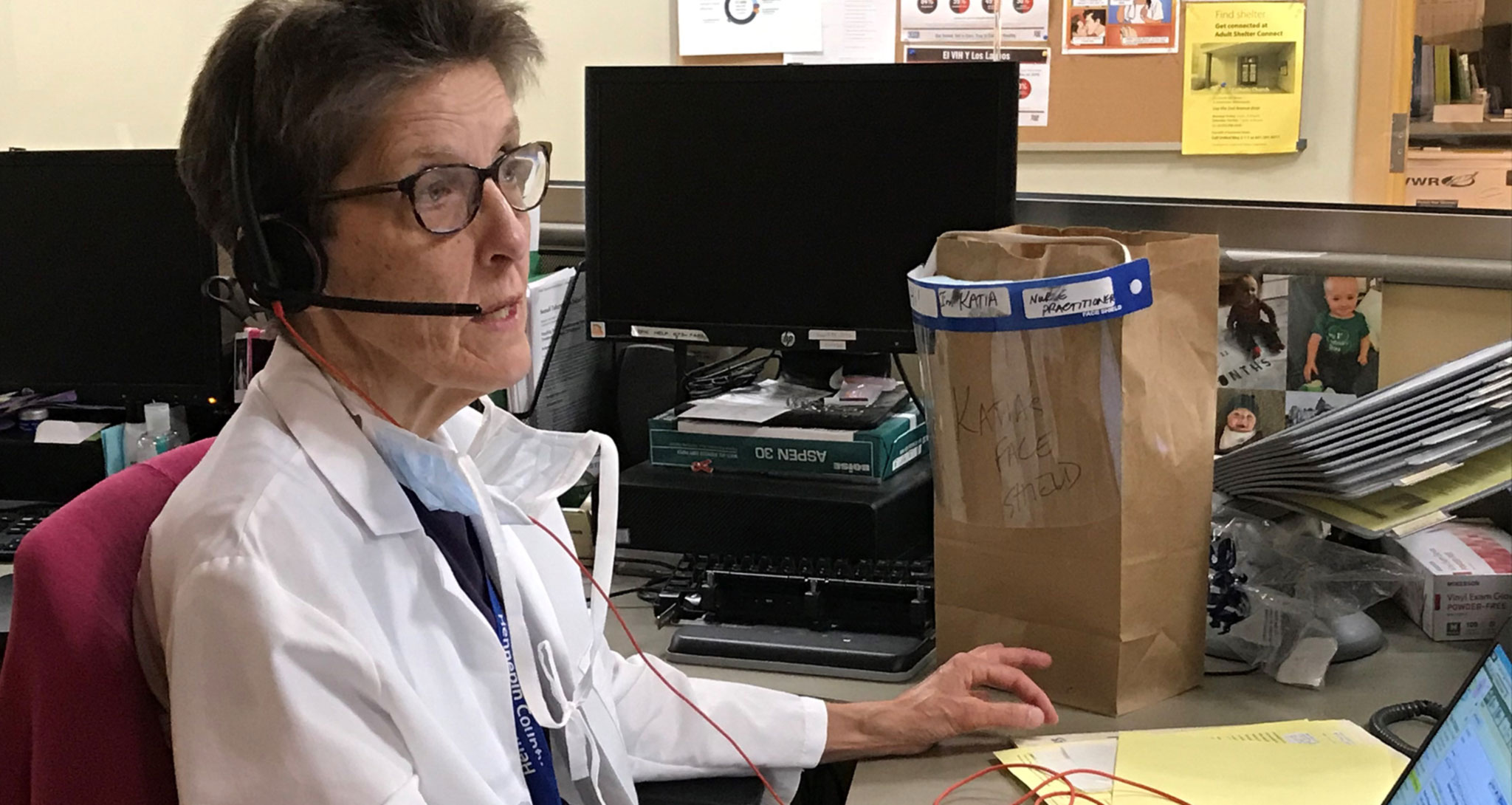
Being at home on the phone is a radically new way for me to deliver care,” says Nurse Practitioner Kathleen McDonough, a long-time provider at the clinic.
“Initially, as a provider, telehealth felt odd,” she says. “But with time and my own adaptations, I think it’s become an even more meaningful way to connect with people.”
For example, McDonough has noticed that some patients feel less shame when they’re talking to a provider over the phone and open up more.
And the new model has also made it easier to engage some clients more holistically. “I’ve reached out to people to ask them not only how they’re doing in a physical sense, but to ask, during this tumultuous time, if they’re safe in their homes, if they feel connected and supported in their communities,” she says.
“This is a teaching moment,” said Clinical Nursing Supervisor Conard Simba. “We’ve learned how do some services more effectively.”
Within the refugee and tuberculosis clinics, one innovation that’s been effective is mailing medications to patients versus having them pick them up.
"We're getting a better response from patients [with transportation barriers] because they don’t have to figure out how to get to the clinic,” says Simba. They’re more compliant when they can get their medications mailed to their home and talk to us on the phone.”
Simba says another teaching moment has been learning how to do his colleagues’ jobs. With staff deployed to respond to COVID-19 outside the clinic, others have cross-trained on different roles. “It’s been a challenging time but I’m very, very proud of the staff we have in the clinic,” says Simba. “They’ve been able to adapt. It’s come to a point where people really appreciate what other people do.”
“This is a really cool clinic with a bunch of dedicated, outspoken, passionate staff who are interested in improving the health of the community,” says McDonough. “We want people to know we’re open; we’re just operating differently. Call us and we’ll figure out a way to help you.”
For an appointment call: 612-543-5555
Written by: Lori Imsdahl